Vasectomy
Vasectomy is one of the safest, simplest and most effective methods of contraception. The intention of a vasectomy is to render a man sterile and no longer capable of fathering further children. We offer a no-scalpel vasectomy (NSV).
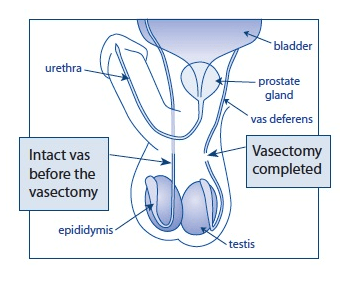
The procedure entails the removal of a portion of the tube (vas deferens) that carry sperm from each of the testicles to the penis. This means that sperm are no longer able to travel from the testicles to the penis, and the man is no longer able to conceive children.
The specialist ‘minimal access’ (no scalpel) techniques used by the experienced Bristol Urology Associates
surgeons enable the operation to be completed in just a few minutes, with the minimum of discomfort during or after the operation. The whole visit to the clinic should take about an hour. No further visits are needed, unless a particular problem arises.
Follow-up specimens for semen analysis will be required. The vasectomy only becomes effective when the ‘sperm reservoirs’ become depleted, after which we will give you the ‘all clear’.
Vasectomy is a permanent method of contraception that is sometimes called “male sterilisation”. Vasectomy is only suitable for those men who are certain, under any circumstances that they do not wish to father any more children.
Suitability for Vasectomy
It is essential for you to have given serious thought about the implications of your decision and be certain that you have had all the children that you will ever want. The vasectomy procedure must be seen as permanent and irreversible. For these reasons we give you (and your partner, if present) the opportunity to discuss with the Consultant prior to the operation, all the implications of the procedure and its permanency.
A vasectomy does not affect a man’s sex drive or ability to enjoy sex. He will still have erections and produce the same amount of fluid when he ejaculates. The only difference is that the fluid will not contain sperm. The body will still produce sperm, but they can’t travel to the penis and are naturally reabsorbed.
Research shows that vasectomy is a very reliable form of contraception. In a recent study of 1000 men, only 20 had positive semen tests (that contained sperm) during a three year follow-up of their vasectomy. Most of these positive results showed low levels of sperm, and many men were negative when re-tested. There were no unwanted pregnancies in the couples studied. However it’s estimated that pregnancy does occur after about 1 in 2,000 vasectomies.
There are many different types of contraception. Before deciding on vasectomy, it is worth discussing the options. Couples also have the option of female sterilisation, although this surgical procedure is not as simple to perform, has more risks than vasectomy and requires a general anaesthetic.
Please be sure that you have read and understood all the literature you have been sent. The surgical techniques that we use do not require the area to be shaved. We recommend keeping the small skin ‘access point’ dry for three days after the operation.
What to expect
You are advised to have a bath/shower beforehand. Please bring or wear tight, well supporting underwear such as Y fronts or briefs to hold the dressing in place and provide additional post-operative support.
Most men are quite capable of driving home after the procedure. However, if you have a tendency to feel dizzy or faint after visits to the doctor or dentist, you are advised to arrange for someone to drive you home.
If your job involves heavy manual work or much lifting, we advise you to make arrangements (with your employer if necessary) to undertake only light duties during the week following your operation. If you are taking any medication which might affect blood clotting such as Warfarin, Aspirin or Clopridogrel you should ensure that the clinic is informed well before you attend your appointment. You should also inform us if you have a valvular or congenital heart condition as you may require antibiotic prophylaxis. We would appreciate if patients with well-known blood-borne infections such as hepatitis could let us know via the booking form.
Prior to your vasectomy operation, you will have a consultation with the doctor who will discuss with you (and your partner if they accompany you), all aspects of the vasectomy and its affects, and will answer any questions you may have. Arrangements with regards to sample collection and post-operative care will also be explained.
You will be asked to sign a consent form which will have been sent to you beforehand; there is space on the form for your partner to sign, should you both wish, but this is not compulsory.
It may be possible for your partner to stay with you throughout the whole operation should you wish; however this is at the discretion of the surgeon, so we suggest you discuss this with the counsellor beforehand.
Vasectomy is routinely performed with a local anaesthetic as a day case, with no need for an overnight stay in hospital. (A general anaesthetic may be given, but this is uncommon.) There is no need to go without food and drink if a local anaesthetic is used. The procedure lasts about 15-30 minutes.
The actual sperms make up approximately 5% of the fluid ejaculated in the semen. The purpose of the operation is to prevent sperm from being present in this fluid. To achieve this, it is necessary to seal the tubes (vas deferens) which carry the sperm to the prostate and seminal vesicles which produce most of the fluid making up the semen.
The skin of the scrotum is first cleaned with a sterilising solution. The doctor injects a small amount of local anaesthetic into the skin of the scrotum (the sac holding the testicles) and the tubes well above the testicles (not the testicles themselves). This rapidly numbs the area after some initial stringing and you will remain awake and able to talk to the doctor if you wish.
A single tiny puncture of 3-5mm is made into the skin and the tubes (vas) are located and sealed using a cautery fusion technique. A short section of each tube is removed to enhance the effectiveness of the technique. No internal or external stitches are used. A small non-adherent dressing is applied to the incision site, held in place by your well-fitting underwear.
We understand that for many men, this will be the first time they have had an operation. The doctor performing your procedure will do his best to help you relax and will talk to you throughout the procedure.
As the local anaesthetic wears off, the scrotum might feel sore and bruising may develop. Occasionally, if the surgeon has difficulty finding both the vas deferens, the bruising can be quite severe. A painkiller such as Paracetamol or Ibuprofen should help relieve any discomfort. Always follow the instructions on the packet.
It is sensible to take it easy for the rest of the day. Most men feel some degree of discomfort during the first few days after the operation, which varies from one individual to another. Again Paracetamol is usually sufficient to relieve any pain. Some men also experience some bruising around the testicles which usually fades after a couple of weeks.
Some men feel fit enough to go back to work the day after their vasectomy (depending on the type of work they do); others may need longer to recover. It is best to avoid heavy lifting or vigorous exercise in the 1-2 weeks after the operation, as this can put a strain on the healing wounds. Wearing tight-fitting underwear day and night for a week after the operation will help to ease discomfort and prevent swelling.
Although most normal activities can be resumed shortly after the operation, we advise all men to take things easy. Sexual activity can be resumed as soon as you feel it will be comfortable, however, we do advise you to wait a few days.
It is fine to have a bath or shower as normal, but the area should be dried gently and thoroughly. Any dissolvable stitches will disappear on their own after about a week, and adhesive strips can be peeled off after 7-10 days.
The wounds should heal fairly quickly. However, if there is an increase in swelling, or if either of the wounds becomes red or hot, the hospital should be contacted immediately, as this indicates that there may be an infection. A small painless lump (less than the size of a pea) may develop at the operation site and may persist for a while. This is caused by the body’s natural healing reaction and no specific treatment is required.
After the operation, there will still be some sperm in the tubes and it will take quite a number of ejaculations to clear the sperm. This can take a few months.
It is therefore essential to continue using an alternative method of contraception until you are informed by us that your system is clear of sperm.
We require you to provide us with samples of your semen at 16 & 18 weeks post-operatively, after a minimum of 24 ejaculations. (Please also see BUA leaflet ‘Vasectomy Aftercare and Semen Samples: What to Expect After your Vasectomy’). On occasion, several more tests may be required until the system is free of sperm. If this should happen, we will advise you accordingly. In rare cases (approximately 1:200), the ends of the tubes may not completely seal or may grow back together again. This usually happens in the first three months and would be detected by semen analysis. Spontaneous re-joining of the tubes can occasionally happen even after your tests have proved negative, sometimes years later. The risk of this happening is approximately 1:2000.
Once we have a semen sample free of viable sperm, we will inform you (by post) of the vasectomy success. Once you have received this confirmation, it will not be necessary to use further contraception. The letter will be sent to you approximately 4 weeks after the second sample has been received.
Specific complications of vasectomy are rare, but can include the following problems:
- Bleeding can occur inside the scrotum, causing it to swell and become painful. This is called a haematoma.
- It is possible for sperm to leak out of the cut tubes and collect in the surrounding tissues. If this happens, hard lumps, called sperm granulomas can form. This is rare but can be painful, and some men opt to have these lumps removed.
- Very occasionally, the cut tubes become inflamed and cause other tubes next to the testicles to swell. If this happens, it can cause a dull ache in the testicles that can last for several months.
- A small proportion of men experience pain for longer. This may be due to pinched nerves or scarring and might require further surgery.
- Very rarely, even when performed correctly, there is a very small risk the tubes can re-join naturally and the man will become fertile again (1 in 2000 men).
Complications, although uncommon, can occur with any surgical procedure, however minor. If you become worried about anything, please contact your GP.
The initial risk that the operation has not worked is 1:100 men. This will be picked up by the samples that you give us. If this occurs the operation will need to be repeated. Once the operation has been confirmed as successful, the risk of pregnancy is 1:5000 after 10 years.
If you think that there is a chance that you will change your mind in later life as a result of changed circumstances, we strongly advise to postpone any decision until you are 100% sure that you want no more children under any circumstances. You may have heard that some men have had a successful reversal procedure; however these are often unsuccessful, may involve significant complications and are very rarely funded on the NHS.
If you are suffering with any personal or sexual problems, then you are strongly advised not to undergo vasectomy until those issues are fully resolved.